Why Value-Based Care is the Key to Addiction Treatment
Why Value-Based Care is the Key to Addiction Treatment
Over 21 million Americans struggle with an active addiction but only 11% will receive treatment. There are many reasons for this including cost, stigma and accessibility. That’s why there’s been more of an emphasis on value-based care in recent years.
11%
Will actually receive treatment
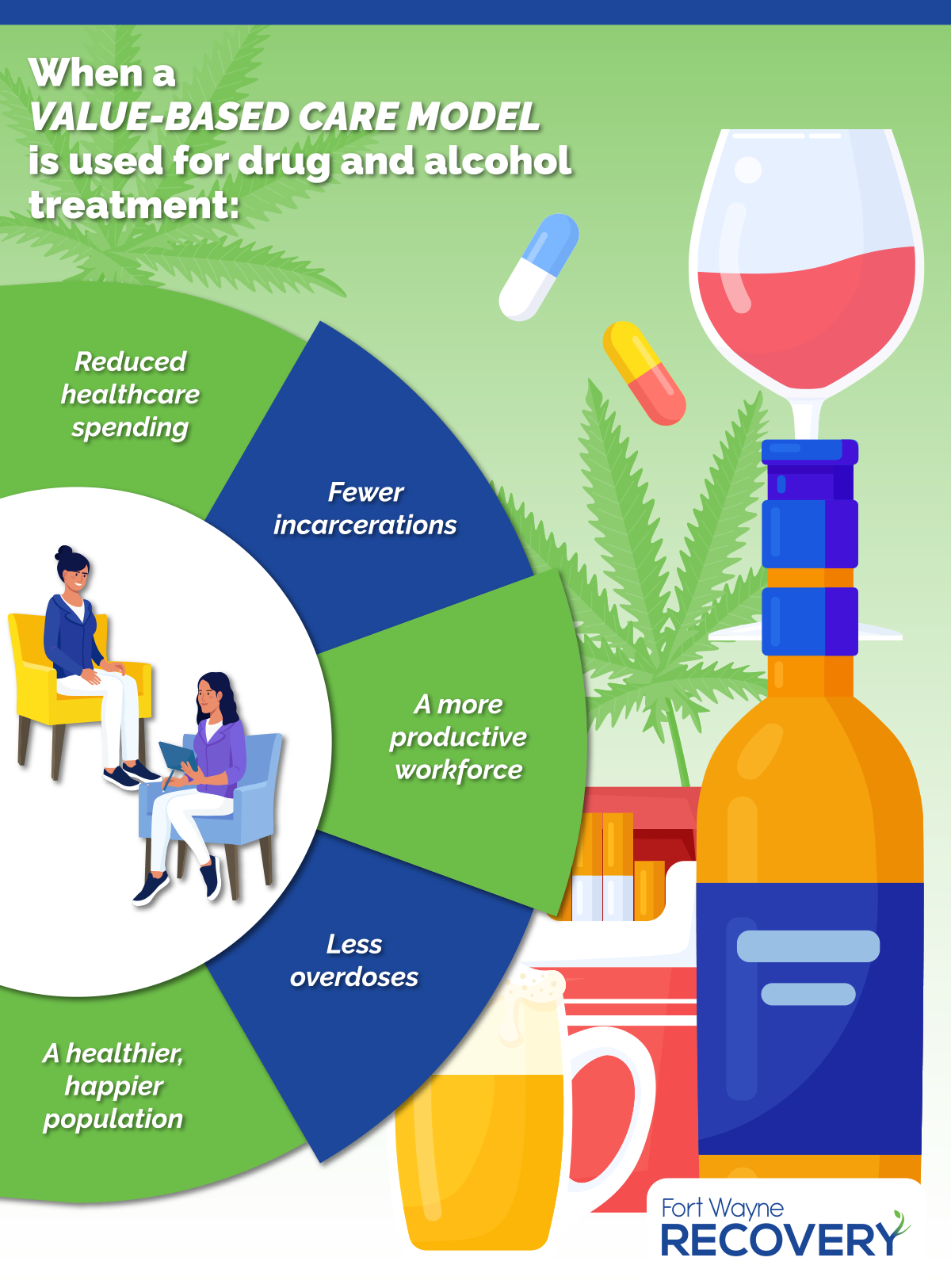
Value-based care focuses on achieving better patient outcomes by emphasizing the quality of medical care versus the number of patients treated. More healthcare providers are advocating for substance abuse disorders to integrate into this model to increase both patient engagement and sobriety rates. Other benefits that come from implementing a value-based model include improvements in physical and mental health, lower healthcare costs and crime reduction.
Value-Based Care Models Focus on Filling Gaps
Value-Based Care Models Focus on Filling Gaps
In the United States, treatment for substance use disorders is expensive and depending on the type of treatment can range from $15,000 to $27,000. This can be cost-prohibitive for individuals who lack medical coverage. Medicaid does not cover residential treatment and only about 60% of employer-sponsored health plans cover addiction medications. Even when insurance covers treatment, people often have to wait for authorization requirements which delay or limit treatment.
There’s also a disconnect between mainstream medicine and substance abuse treatment. In a survey, only 1 in 4 medical practitioners said they’d received any addiction training during their medical education. This lack of education is problematic when physicians don’t know how to properly incorporate treatment for substance abuse with other medical conditions such as pregnancy. One study found that some doctors may be less likely to prescribe opioid agonist therapies (OATs) to treat opioid addiction during pregnancy even though OATs are safe and work well during pregnancy.
Alicia Wells, Director of Public Relations for Fort Wayne Recovery and Allendale Treatment knows this all too well. She said that she had a negative experience when she went to the hospital in labor and was on an OAT for an opioid use disorder. “The hospital I gave birth at was Catholic and didn’t understand that there were certain types of medications that I shouldn’t be on and it reversed my OAT so I started going through withdrawal while I was in labor,” says Wells. “After I gave birth, I felt an immense amount of stigma from one of my nurses who contacted CPS when she realized I was on medication for my substance use disorder. Part of my work now with Bare Knuckle Recovery is finding medical practitioners who understand what people with substance use disorders are going through so they can provide them with better care through their recovery.”
“The hospital I gave birth at was Catholic and didn’t understand that there were certain types of medications that I shouldn’t be on and it reversed my OAT so I started going through withdrawal while I was in labor.”
“The hospital I gave birth at was Catholic and didn’t understand that there were certain types of medications that I shouldn’t be on and it reversed my OAT so I started going through withdrawal while I was in labor.”
A Better Patient Experience Leads to Better Outcomes
When implemented into a care plan for a patient struggling with a substance disorder, the value-based model creates a personalized treatment plan that integrates primary care, behavioral health, detox, medication and group therapy where practitioners work together to provide a better patient experience. This method has been shown not only to be successful in traditional healthcare models but research shows that a longer, integrated substance use treatment plan can improve the patient’s quality of life and reduce overdoses, relapse rates and incarcerations.
Tommy Streeter, a community outreach coordinator for Allendale Treatment and Fort Wayne Recovery says that being in a safe environment where you’re surrounded by medical professionals who can treat both physical and mental ailments during detox makes the process so much easier. “I tried to detox on my own at home and I felt terrible and often found myself ending the process by taking more heroin to make me feel better,” says Streeter. “Detoxing on your own is a difficult process and having access to a treatment program where you’re surrounded by medical professionals who can make the process easier, is a much safer and better experience.”
Saving Money While Saving Lives
Another benefit of using a value-based care model to treat substance use disorders is that it could help save a substantial amount of money. Substance disorders cost the American economy $740 billion annually in healthcare expenses, lost workplace productivity and crime-related costs.
When people engage in ongoing drug and alcohol abuse, it’s going to start taking a toll on their health. Years of heavy drinking can cause liver disease and certain cancers. Ongoing marijuana use can lead to chronic bronchitis and the use of stimulants such as cocaine and heroin can cause heart disease. All of these conditions mean more trips to the doctor and medications to manage them, which can be taxing on the American healthcare system. Substance abuse can also cause more trips to the emergency room when people overdose. In 2021 alone, there were over 107,000 fatal overdoses in the United States.
“I was at my girlfriend’s house and told her I was going to take a shower and that’s when I overdosed in the bathroom.”
Nate Moellering, A Community Outreach Coordinator
Nate Moellering, a community outreach coordinator at Allendale Treatment and Fort Wayne Recovery says that he was lucky he didn’t lose his life overdosing twice on the same day. “I was at my girlfriend’s house and told her I was going to take a shower and that’s when I overdosed in the bathroom,” says Moellering. “I remember waking up with firefighters standing over me. They put me in an ambulance and took me to the hospital. I didn’t stay long because I left against medical advice and 6 hours later, I was back at her house after I had scored some more heroin and overdosed again. EMS had to be sent out to her house twice to revive me in less than 24 hours.”
Substance abuse in the workforce can cause a variety of problems including workplace accidents, employee absenteeism, decreased productivity and conflict with other employees. A national survey reported that 15.3% of workers admitted to working under the influence of alcohol. This has led to more employers embracing value-based care models to expand on substance abuse treatment and behavioral health services for employees.
Incarceration rates could also decrease from a value-based care model. 85% of the prison population has an active substance use disorder or were incarcerated for a crime involving drugs or drug use. Prisons often fail to provide any substance abuse treatment and the ones that do, often only provide medication-assisted treatment (MAT) and no mental health counseling. This means that once an inmate is released from jail, they will often continue to engage in their substance use disorder and stay trapped in the cycle of drug use driving up crime and incarceration rates.
By focusing on creating a comprehensive healthcare approach for people struggling with a substance abuse disorder, the value-based care model can help more people overcome their addictions while also creating a healthier, safer and more productive society.

